Degenerative Disc Disease
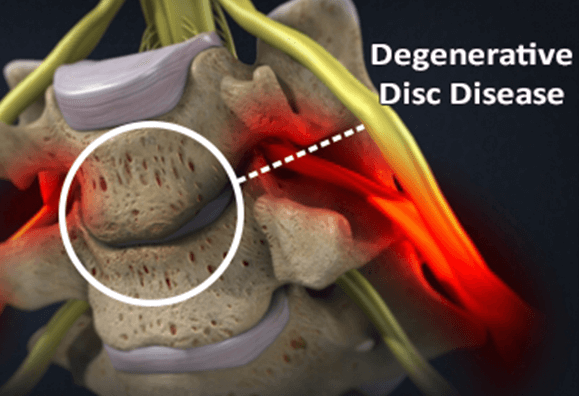
Degenerative disc disease is not necessarily a disease but is instead a term used to describe changes in the spinal discs as we age. When the spinal discs lose their water content, they become smaller and bring the vertebrae closer together, which narrows the nerve openings in the spine. Ultimately, all of these changes lead to less shock absorption when you walk, run, and jump.
What Is Degenerative Disc Disease
Over time, the discs gradually deteriorate due to age, infection or injury. The gelatinous material may lose its ability to absorb water and the thick coating may weaken, stiffen, bulge or rupture. The once flexible, supple disc becomes stiff and rigid, losing its cushioning ability and restricting movement. A disc that is compromised and impinges on nerves in the spinal column can result in pain.
Degenerative disc disease describes these changes, some of which can lead to certain spine conditions, including:
- Bulging disc
- Spondylosis
- Pinched nerves
- Foraminal stenosis
- Radiculitis
- Sciatica
- Cervical or lumbar spinal stenosis or spondylolisthesis, or the narrowing of the spinal canal
- Osteoarthritis, the breakdown of the cartilage that protects and cushions joints
What Causes Degenerative Disc Disease?
Degeneration of the spinal discs is a normal part of the aging process, which may result in degenerative disc disease. These age-related degenerative disc disease causes may include:
- The loss of fluid in your discs, reducing the capability of the discs to act as shock absorbers and making them less flexible
- Tears or cracks in the annulus allow the jelly-like material inside the disc to bulge, rupture or break off fragments of bone
Are You at Risk for Degenerative Disc Disease
These changes are more likely to occur in smokers or those who do heavy physical work, such as repeated heavy lifting. People who are obese are more likely to have degenerative disc disease symptoms. A sudden injury leading to a herniated disc may also begin the degeneration process.
How Does the Spine Degenerate?
The degeneration of the spine involves the gradual loss of normal spinal structure and function. With aging, this loss can be gradual. Repeated strains and sprains or overuse of back, for work or through sports, can cause the gradual degeneration of the discs.
When you’re young, the discs are soft and supple. With age, the discs erode and become drier, which reduces their ability to absorb weight and act as a shock absorber during everyday activities.
Through injury, infections or even arthritis, the degeneration process may occur at a faster pace than normal.
It is expected that by age 40, everyone will experience some disc degeneration. However, some may not experience the symptoms associated with degenerative disc disease until long after the discs have begun degenerating. One study estimated that about 75% of participants under the age of 50 has disc degeneration while more than 90% of people over the age of 50 showed signs of degeneration.
Types of Degenerative Disc Disease
There are three types of degenerative disc diseases and they are named for the area of the spine they affect: cervical, thoracic, and lumbar. Cervical disc disease, the second most common type, occurs when a disc in one of the neck vertebrae degenerates. The most common type of disc disease occurs when one or more discs degenerates in the lumbar spine. Thoracic disc disease (the least common) occurs when a disc in the thoracic spine degenerates. Several types of disc deterioration symptoms can occur, depending on the location of the affected discs.
Cervical Disc Disease
Cervical disc disease involves the degeneration of one or more of the discs in the cervical spine. According to the study noted above, cervical disc degeneration was more prevalent at the C5-C6 level. For those suffering from cervical disc degeneration disease, they may experience neck pain, nerve pain that radiates down to the shoulders, arm, hand or fingers. Neurological symptoms, such as tingling, numbness or weakness can also radiate down into the upper extremities.
If the pain subsides, it could be a sign of degenerative cervical disease. However, these symptoms can become chronic as the disc continues to deteriorate.
Thoracic Disc Disease
Thoracic degenerative disc disease is the degeneration of the thoracic spine, which consists of 12 thoracic vertebrae numbered T1 to T12. Disc degeneration in the thoracic spine, or mid-back at the level of the ribcage, is rare. However, when it does occur, back pain is often located around the site of the degenerated disc.
Lumbar Disc Disease
Lumbar disc disease involves the degeneration of spinal discs in the lumbar spine. The low back pain often associated with lumbar disc disease may be caused by inflammatory proteins in the disc space that irritate the surrounding nerves or when the annulus is worn down and can no longer absorb the stress of the spine.
People with lumbar disc disease may experience low back pain anywhere between the ages of 20 and 50. Some may experience pain that is made worse when sitting or bending, deep aches in the low back that worsens, and pain radiating down into the hips, thighs and legs.
Although low back pain is common, anyone experiencing pain that doesn’t subside after a few days or worsens over time should get be evaluated by a doctor.
Symptoms of Degenerative Disc Disease
Degenerative disc disease symptoms vary from person to person. Many people have no pain, while others with the same amount of disc damage have severe pain that limits their activities.
In general, symptoms include:
- Chronic pain in the neck and/or back
- Severe episodes of pain that can last weeks or months
- Difficulty with prolonged sitting or standing
- Sporadic tingling or weakness
- Pain that worsens when sitting, bending, lifting and twisting
Diagnosing Degenerative Disc Disease
Through medical history and a physical examination, a doctor can determine if degenerative disc disease is the cause of your back pain.
A doctor will ask about your symptoms, any injuries or illness that may have caused disc degeneration, and what activities are causing pain. During the physical examination, the doctor will examine your flexibility, range of motion and look for any areas of nerve-related changes or tenderness.
Although a physical examination can help with a diagnosis, imaging tests such as an x-ray, MRI scan, CT scan or myelography may also be requested to determine if there is radiculopathy, nerve damage, facet joint hypertrophy (enlargement), or loss of water in a disc.
Treatment for Degenerative Disc Disease
Degenerative disc disease treatment will vary depending on the severity of your symptoms and how much they impact your day-to-day life. Patients who have been diagnosed with degenerative disc disease may begin with conservative treatments, which could provide pain relief, however, depending on the degeneration and level of pain, additional treatment including degenerative disc disease surgery may be required.
Non-Surgical Treatment
Non-operative care will involve a combination of non-invasive treatments that include physical therapy, pain management and clinical medicine to reduce musculoskeletal pain and increase your mobility. Some treatment plans may include:
- Back braces
- Spinal manipulation
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Exercise plans
- Hot/cold therapy
Steroid injections can also deliver medication directly into the affected area to reduce inflammation. For many with disc degeneration, a regiment of a combination of therapies may be suggested.
Surgical Treatment
If you have been diagnosed with DDD, you may be a candidate for the patent protected Bonati Spine Procedures. The Bonati Spine Institute has been performing advanced spine surgery for decades, and with over 75,000 successful procedures performed, it is the world leader in advanced spine surgery.
The Bonati Spine Procedures offer an array of surgical techniques to treat degenerative disc disease when conservative treatments such as exercise and physical therapy do not offer pain relief.
These procedures may include:
Discectomy
A discectomy is a surgical procedure performed to remove a portion of a bulging or herniated disc which is pressing on the spinal cord and/or spinal nerve roots.
Laminectomy/Laminotomy
A laminectomy/laminotomy is a decompressing surgery that relieves pressure on the spinal nerves. This procedure is performed one vertebral level at a time, to address the primary cause of the pain first. A laminectomy/laminotomy is performed through a small opening through which a series of tubes are introduced to accommodate surgical tools and imaging equipment. The lamina is then accessed through an arthroscope, and small portions of the lamina are removed to release the pressure from the spinal nerves.
Foraminectomy/Foraminotomy
Foramina are small openings present between every pair of vertebrae in the spine. If a part of the foramen is pressing on a nerve as it leaves the vertebral opening, a foraminectomy/foraminotomy may be performed. This procedure uses local anesthesia and conscious IV sedation to allow surgeons to target the source of the pain with precise accuracy. The tissue compressing the nerves is removed with a set of surgical instruments inserted through a very small incision.
Facet Thermal Ablation
A Facet Thermal Ablation is a laser eradication of sensory nerves causing pain.
Laser Debridement
Debridement is the surgical removal of torn, inflamed, contaminated, damaged or dead tissue. Debridement may be completed in the lumbar, thoracic or cervical spine. Laser debridement involves using a laser to obliterate the tissue.
The Bonati Spine Institute is proud to have completed over 75,000 successful procedures with a 98.75% patient satisfaction rate with no hospital stay and rapid recovery time. Treatment of degenerative disc disease starts with a visit to The Bonati Spine Institute.
Prevention and Self-Care
Although degenerative disc disease is associating with the aging process, there are some changes that can be made to prevent painful and incapacitating symptoms.
- Exercise
- Eat well
- Learn and use correct lifting techniques
- Sleep on your side to put less pressure on your spine
- Reduce alcohol consumption
- Quit smoking
- Maintain a healthy weight
Other lifestyle modifications like changing your daily work routine if you’re repeatedly exposed to significant back stress may also help as can maintaining proper posture.
Common Questions
Whether you’re researching degenerative disc disease or have recently been diagnosed, you may have many questions. Below are some common questions about the disease.
Can I treat the disease on my own
There are several things you can do to relieve pain from degenerative disc disease, such as stretching, resting, using a cold pack, and taking over-the-counter pain relievers. However, if the pain worsens or becomes chronic, you should see a doctor in order to create a treatment plan.
How long will it take to recover
There is no cure for degenerative disc disease. Continued treatment can help lessen the pain and surgery can help those suffering from debilitating pain.
Does the disease spread through the spine?
Because degenerative disc disease is only a term used for the condition, it cannot spread down the spine. However, those with weak vertebral discs may be more prone to injury or additional degeneration, which can lead to problems in other areas or levels of the spinal column.
If you have been diagnosed with degenerative disc disease and believe you may be a candidate for surgery, contact the professionals at The Bonati Spine Institute to receive a review of your MRI.
See how The Bonati Spine Procedures helped those with Degenerative Disc Disease by clicking here.
