Is there help for arachnoditis? If you go to any doctor’s office, especially radiologists and anesthesiologists, and ask them about Arachnoiditis, you will likely be told that it does not exist, it is an urban myth, no one knows anything about it and that it is not a painful condition. Do an internet search on Arachnoiditis and you may find dozens of theories as to its cause.
Dr. Charles Burton, the founder of the North American Spine Society and the world’s leading expert on this condition noted in a report that, “despite the availability of a wealth of published scientific information on the subject, it has not been well appreciated by the medical profession that the advanced forms of Arachnoiditis may be associated with incapacitating pain and disability. Arachnoiditis represents a worldwide public health problem of considerable magnitude.”
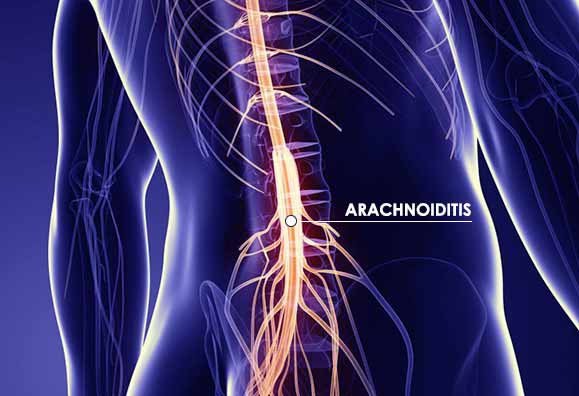
Adhesive Arachnoiditis is an inflammation or irritation of the arachnoid membrane of the meninges. The meninges are a three-layer tissue covering around the spinal cord, spinal nerves and the brain. The arachnoid membrane is the middle layer of this covering. As with most inflammatory conditions, when the arachnoid membrane becomes irritated it can cause pain. This irritation may occur when the spinal cord gets compressed, whether by injury, chronic spinal stenosis, degenerative conditions such as bone spurs, leaked disc material (which is known to be highly irritant to nerves), or a spinal procedure, such as an epidural steroid injection or “open” fusion spine surgery.
In Adhesive Arachnoiditis inflammation leads to scar tissue formation. Scar tissue, in turn, can cause spinal nerves to stick together inappropriately. This clumping tends to occur in the area just on the inside of the spinal nerve roots , just prior to where they begin to branch out and develop into peripheral nerves, the nerves that enable you to feel, respond and move.
The primary cause of Adhesive Arachnoiditis can be traced back to Lumbrosacral Spinal Stenosis, also known as lumbar spinal stenosis or lumbosacral nerve root compression. These terms describe arthritis of the joint between the last lumbar vertebra and the sacrum, which is one of the bones that makes up the pelvis. This arthritis narrows the canal through which the spinal cord and nerves pass. The intervertebral disc between the vertebra and the sacrum is often degenerated, further narrowing the canal. Symptoms may include nerve sensations such as stinging, tingling, numbness or burning in the low back and legs.
Adhesive Arachnoiditis does not respond to the many available traditional “conservative” treatments. Reaching the arachnoid space without doing further damage to it makes invasive type treatment, such as “open” spine surgery, precarious. Invasive “open” spine surgery results in more scar tissue formation in the space.
The idea behind treatment for Adhesive Arachnoiditis is to relieve pressure from scar tissue in the arachnoid space. The Department of Neurosurgery at University Hospital, Groningen, The Netherlands, in a study entitled “Spinal Arachnoiditis: Disease or Coincidence?” states that “It has been demonstrated that there are patients with Arachnoiditis and concomitant herniated disc disease or lumbar stenosis who improved completely after surgical management of the latter conditions”.
“Open” fusion surgery can cause aggravation to the current symptoms. It is not as effective as a minimally invasive Foraminoplasty in addressing the effects of Adhesive Arachnoiditis. A Foraminoplasty is carried out in the gaps or ‘foramen’ between the vertebrae, allowing the nerve to be thoroughly liberated.
Single closely targeted surgery enables Adhesive Arachnoiditis sufferers to be precisely treated with minimum of damage to tissues, reduced risk and enhanced long-term outcome without the use of general anesthesia. This is only possible by the use of Endoscopic Minimally Invasive Spine Surgery where the full length of the exiting nerve can be explored and the points of irritation clearly demonstrated. Minimally Invasive Endoscopic Lumbar Decompression and Foraminoplasty have achieved great success in decompressing the Arachnoid nerve sac.
Help forArachnoiditis
The Bonati Spine Institute pioneered the development of minimally invasive endoscopic surgical procedures, and we have performed more than 70,000 successful procedures to treat Lumbrsacral Spinal Stenosis and other degenerative spine conditions. These exclusive patented procedures minimize the risk for subsequent scar tissue formation, even when used in treating problems from failed previous “open” spine surgeries. If you are planning on having spine surgery, choosing to go minimally invasive will reduce your risk for excess scar tissue formation, and hence, reduce your risk for Adhesive Arachnoiditis.