The blog is excerpted from VeryWell Heath article b Anne Asher, CPT and m Scott Sundick, MD
Revision spine surgery may be deemed necessary by your doctor (or you) if you still have symptoms after the first procedure, or if you have new symptoms. But how do you know if you really need that 2nd back surgery?
Check this list to start your research.
Recurring Disc Herniations
If, after a discectomy, you again have sciatica, pain down your arm, or other herniated disc symptoms, you may have a recurring herniation or cervical radiculopathy. A recurring disc herniation is basically a repeat of the problem that led to the surgery in the first place.
A discectomy typically removes only those pieces of disc material (called fragments) that have become partially or fully disengaged from the main disc. You still have your disc, and it is still possible to herniate the part that’s left.
Pseudoarthrosis
Pseudoarthrosis is a term that describes a lack of bone fusion no later than one year after a spinal fusion surgery.
Pseudoarthrosis is very common, occurring in up to 68% of lumbar fusions, according to Dr. Joshua D. Auerbach, Chief of Spine Surgery at Bronx-Lebanon Hospital Center in New York City. Of these, between 6 and 36% require a re-operation, he says.
Some things that may play a role in the development of pseudoarthrosis after your first surgery include:
- The nature of your original diagnosis
- Type of hardware installed
- Type of bone graft, if any, used
- Your health habits and condition. For example, if you smoke or take corticosteroids, your risk for pseudoarthrosis may be increased.
- If you have a spinal fusion in which no plates, screws or other hardware are installed.
In his chapter on revision lumbar spine surgery for the medical text entitled The Textbook of Spinal Surgery, 3rd Edition, Auerbach cites studies that show fusions performed without the implantation of hardware may increase your risk for pseudoarthrosis by 70%. That number is much lower — 10% — for spinal fusions in which hardware is placed, he reports.
Adjacent Segment Disease
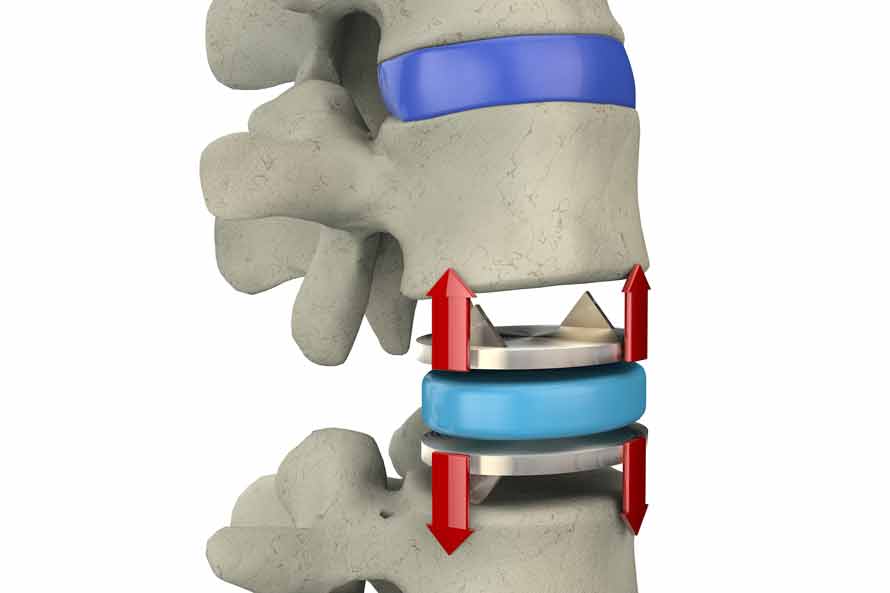
ASD, or adjacent segment degeneration, is a condition in which anatomical changes occur at spinal joints above and/or below the place a back surgery is done.
Auerbach says that biomechanical studies do show extra stress at adjacent levels following a fusion. Because fusion tends to increase the steepness of the angle between the two bones of an intervertebral joint, the way your spine moves will likely be altered. This may impose extra pressure on some areas of the joint. “The discs pick up the slack,” he says.
According to Auerbach and others, this type of increased stress is a big reason why many in the industry are pushing for the development of motion preservation surgical techniques and devices. Advances in technology — for example, total disc replacements — enable doctors to treat the problem without sacrificing movement in the affected area.
In case you are wondering, there are studies that show an advantage to having a disc replacement over a spinal fusion, although not all the questions have been answered (as of 2016). For example, in an analysis of three studies comparing the results of cervical disc replacements with spinal fusion two years after the procedure, researchers found that people who had arthroplasty (disc replacement) were 44% less likely to need a second surgery. That same study did not report on any significant benefit of arthroplasty for minimizing or avoiding ASD, however.
Revision TDR
Total disc replacement, often called TDR for short, is a relatively new surgery (in the United States, at least) that is seen by some spine experts as a viable alternative to spinal fusion surgery. Disc replacements have been done in Europe for a while, but the U.S. is adopting this technology more slowly.
Auerbach says that only about 0-5% of patients referred for spine surgery fit the criteria for a safe and successful total disc replacement procedure. If you are not a candidate, but you have one anyway, he says, you may experience complications.
One of the most common complications leading to a revision TDR (as a second disc replacement surgery is sometimes called) is device failure. Examples of device failure include malfunctioning of the prosthetic disc implanted in your spine, or when the device shifts its position (extrudes).
Problems With Implanted Hardware
One may also run into problems with the hardware that was implanted in your spine. This includes prosthetic discs, as mentioned above, as well as hardware used for spinal fusion and other types of back surgery. The instrumentation, as it is sometimes called, may break, or the surgeon may have placed it in the wrong position during the procedure.
One type of hardware problem resulting from a back surgery is a syndrome known as “painful hardware.” In this case, the implanted items are simply too uncomfortable, Auerbach says.
Frank Cammisa, Jr., M.D., Chief of the Spine Service at the Hospital for Special Surgery in New York says that pain due to painful hardware syndrome usually arises from soft tissue (i.e. your muscles, ligaments, tendons, and fascia). Addressing painful hardware syndrome sometimes requires surgery to remove the offending items.
Find Revision Spine Surgery WITHOUT Hardware
There are many reasons why spinal revision surgery may be required, so it is important to schedule and complete follow-up appointments. If you are experiencing pain, be honest with your doctor about these issues so they can be remedied as soon as possible. The Bonati Spine Institute can examine your MRI and determine if you need spinal revision surgery. The physicians at the Bonati Institute have performed over 70,000 Bonati Spine Procedures, including spinal hardware removal and various procedures for failed back surgery syndrome WITHOUT implanting hardware or devices of any kind. Learn more about how we can help you by calling 855-267-0482 or complete our online contact form here.
Read the full VeryWell Health article here: https://www.verywellhealth.com/back-problems-and-surgery-296527